Oesophageal Cancer is cancer of the oesophagus, also known as the gullet or food pipe.
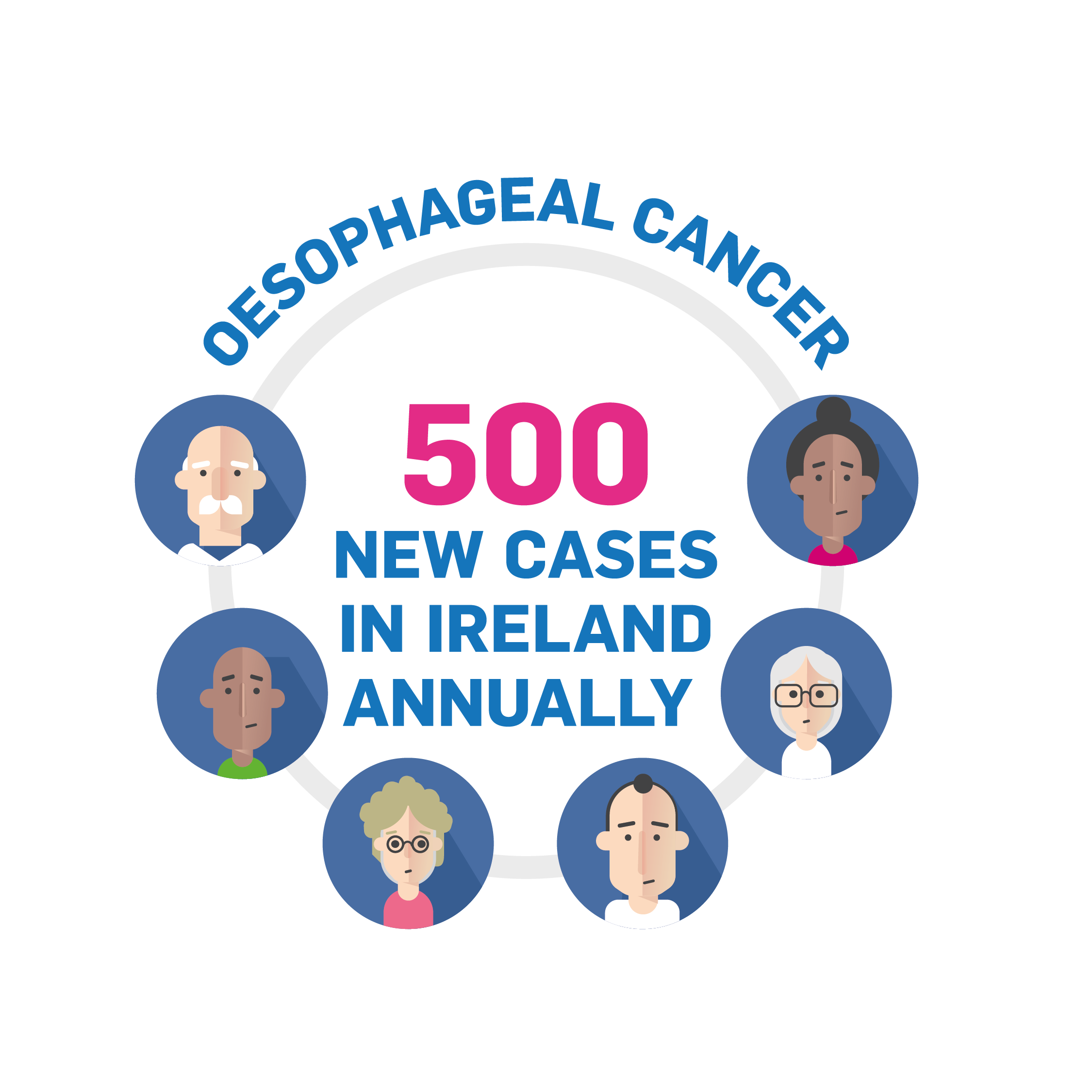
Ireland has approximately 450 to 500 new cases of Oesophageal Cancer annually this is one of the highest rates in Europe.
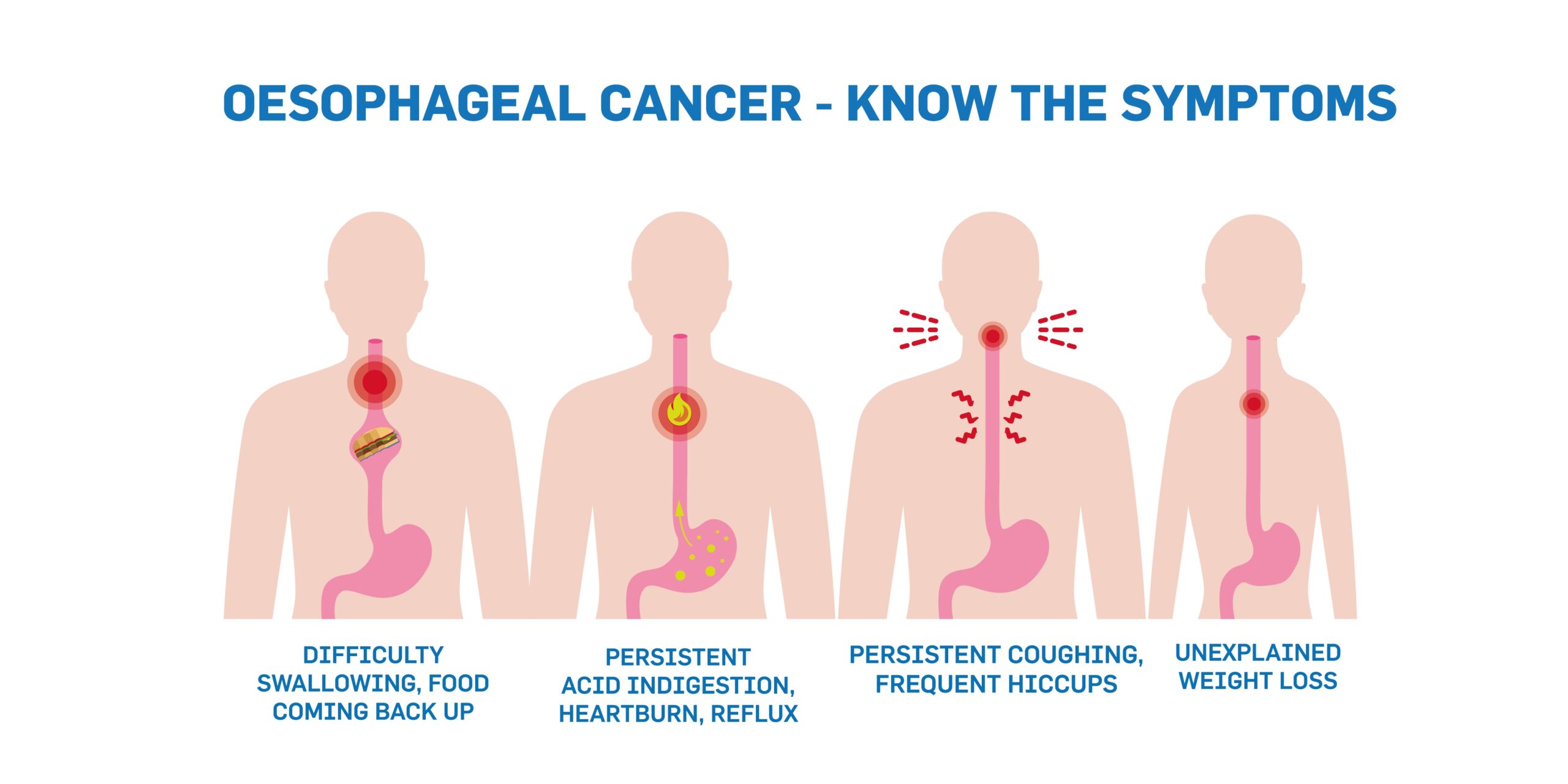
More so than with many other cancers, the early signs of Oesophageal Cancer can be easy to overlook. Many people could be tempted to dismiss what can seem to be digestive complaints.
Early detection is vital so visit your doctor the moment you notice any of these symptoms persisting:
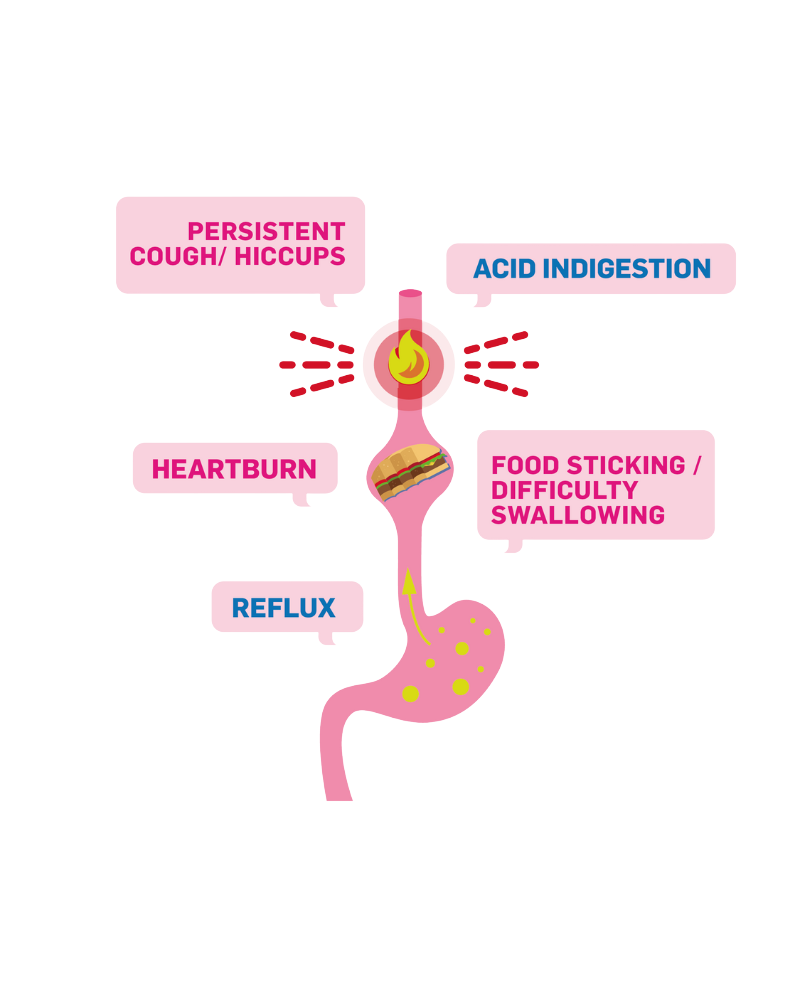
Difficulty Swallowing — feeling that your food is sticking or catching after swallowing
Acid Indigestion or Heartburn that doesn’t go away and can be described as persistent
Food coming back up — either before reaching the stomach (Regurgitation) or after (Vomiting)
Progressive, unexplained and unplanned weight loss
Unexplained anemia
Hoarseness that persists — and isn’t due to a cold
Coughing, Burping, Belching or Hiccups that don’t subside
Other conditions can also account for these issues, but visiting your GP promptly is the best way to find out as early as possible. If you subsequently notice no improvement, follow up with your doctor too, as you may need to be referred to a Gastro-Intestinal (GI) Specialist.
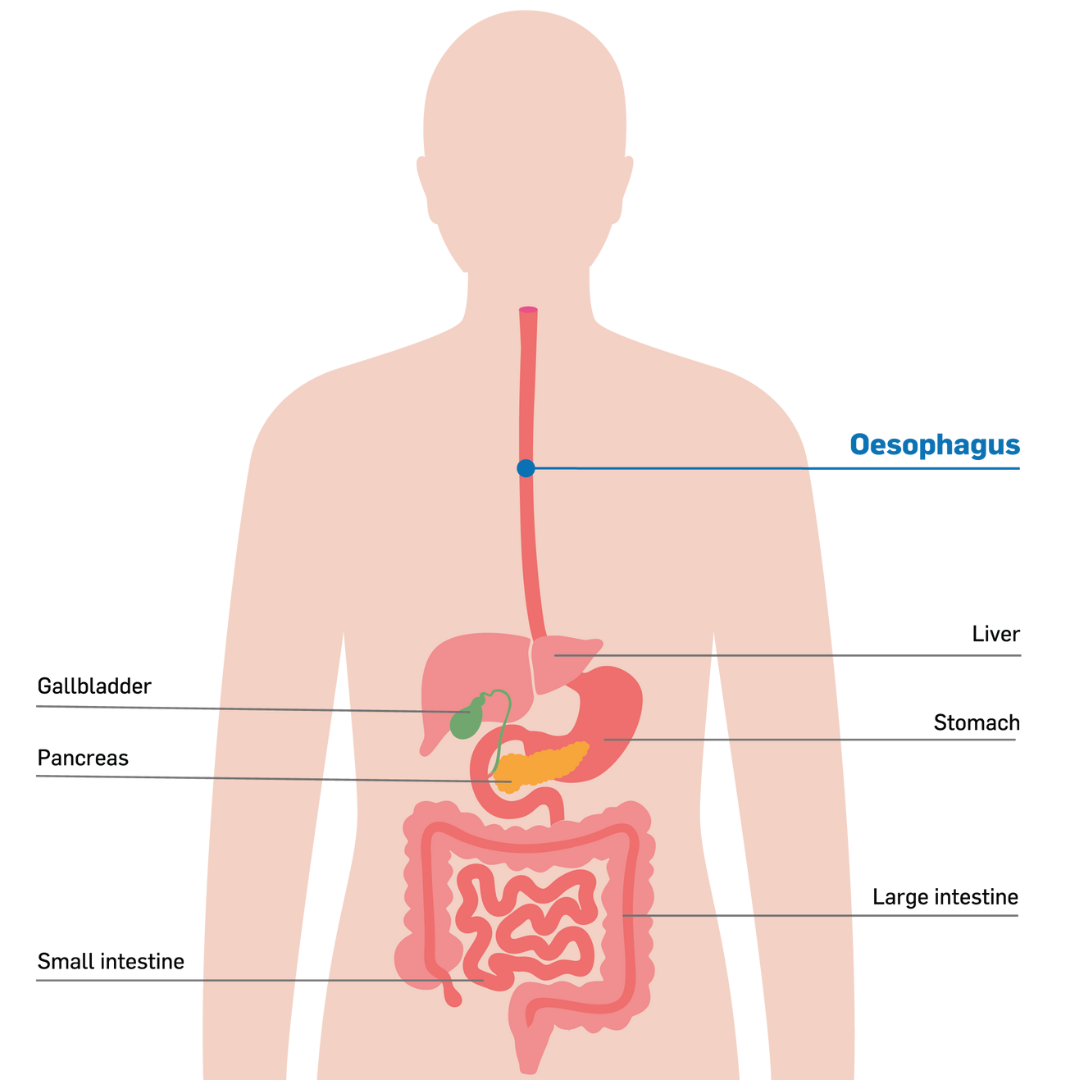
The Oesophagus is a part of the digestive system, a muscular tube that connects your mouth to your stomach and can sometimes be referred to as the gastro-intestinal tract or GI tract. The Oesophagus is usually between 25-30cm in length in adults.
Food and liquid pass through the oesophagus. There is a muscle - the sphincter - at the top of the oesophagus that opens to allow food or liquid to pass to the stomach. This also functions to stop food or liquid from going down the windpipe.
The windpipe or trachea is in front of the upper part of the oesophagus and connects your mouth and nose to your lungs, to allow you to breathe. Below your lungs is the diaphragm, a layer of muscle that helps you to breathe. The oesophagus sits above the diaphragm in your chest.
When you swallow food and liquids, the walls of the oesophagus squeeze from top to bottom to allow the food and liquids to be pushed along the oesophagus in a wave-like motion, moving it to the stomach. This muscular action is known as peristalsis.
These muscles also contract to keep the food and liquids moving in the right direction towards the stomach to prevent food coming back up. The oesophagus joins the stomach at the lower part of the oesophagus at the gastro-oesophageal junction.
There are sphincter muscles close to the gastro-oesophageal junction to control food and liquids moving from the oesophagus to the stomach. This sphincter muscle then closes to stop the contents of the stomach and stomach acid moving backwards from the stomach into the oesophagus.
The oesophagus is made up of four layers:
The inner layer - the mucosa, is a moist layer that helps food to pass easily into the stomach.
The submucosa - a layer of the oesophagus with glands that produce mucus also keeping the oesophagus moist.
The muscular layer - the muscularis squeezes and pushes food down into the stomach.
The outer layer - the adventitia attaches the oesophagus to surrounding parts of the body.
While specific causes of Oesophageal Cancer can be difficult to pinpoint, and Oesophageal Cancer can affect any adult at any life-stage, the following have been identified as key risks, conditions, behaviours and lifestyles that may increase your risk of developing this disease.
Anything that can increase your risk of cancer is called a risk factor. Those that lower the risk are called protective factors. Having one or more risk factors does not mean that you will definitely get Oesophageal Cancer but it is important to be aware of the risk factors.
Obesity
Being overweight can significantly increase your risk of developing Oesophageal Cancer. and also because other factors like long-term reflux, heartburn and/or acid indigestion are more common in people who are overweight.
Persistent Acid Reflux
Acid reflux or heartburn occurs when stomach acid constantly flows back up into the oesophagus. As a long-term, persistent condition, it can damage the oesophagus and in a small number of sufferers, can lead to a pre-cancerous condition called Barrett’s Oesophagus.
Acid reflux affects about 1 in 3 people. It is also known as Gastro-Oesophageal Reflux Disease (GORD).
Smoking
Smoking increases the risk of Oesophageal Cancer. The risk increases the longer a person smokes for and the more they smoke. All types of smoking are very harmful.
Smoking and drinking together further increases the risk of Oesophageal Cancer.
Alcohol
Your risk of Oesophageal Cancer increases if you drink more than 14 units of alcohol a week. Drinking a lot of alcohol over a long period of time also increases your risk of developing Oesophageal Cancer.
People who drink alcohol and also smoke increase their risk of Oesophageal Cancer.
Age
The older you get, the higher the risk of Oesophageal Cancer. This type of cancer is most prevalent among over 60s, and less common for under 40s. However, increasingly we’re seeing this cancer can occur outside these age brackets. It is important that anyone experiencing the symptoms of Oeophageal Cancer seeks advice from their GP.
Gender
Three times more men than women are affected by Oesophageal Cancer, though recently the proportion of women diagnosed in Ireland has risen.
Diet and Nutrition
If your diet is deficient in certain vitamins and minerals such as zinc and riboflavin and vitamins A, C the risk of Oesophageal Cancer can increase. Also Eating lots of red meat and processed foods such as sausages, burgers and ham may increase your risk of developing Oesophageal Cancer.
There is some evidence also suggests that drinking very hot drinks may not be wise, as over time, they can damage the lining of your oesophagus.
Other Medical Conditions
Achalasia is a condition where the muscle that controls the opening between the oesophagus and the stomach doesn’t relax properly. People with achalasia have a higher risk of developing Oesophageal Cancer.
Tylosis is a rare inherited skin condition and those affected are also at risk of developing Oesophageal Cancer.
Barrett's oesophagus
can increase your risk of Oesophageal Cancer, although the risk is still small. Many people with Barrett’s Oesophagus do not develop cancer. Find out more about Barrett’s Oesophagus on the OCF website.
Acid Reflux also known as Gastro - Oesophageal Reflux disease (GORD) increases your risk of developing Oesophageal Cancer. Acid Reflux is a common condition where stomach acid flows back into the oesophagus from the stomach. It is important that if you experience long term symptoms you address these with your GP, the longer that symptoms persist, the higher the risk.
It is important to remember that having a risk factor does not mean you will definitely get Oesophageal Cancer. If you are worried, please talk to your GP and explain your concerns fully.
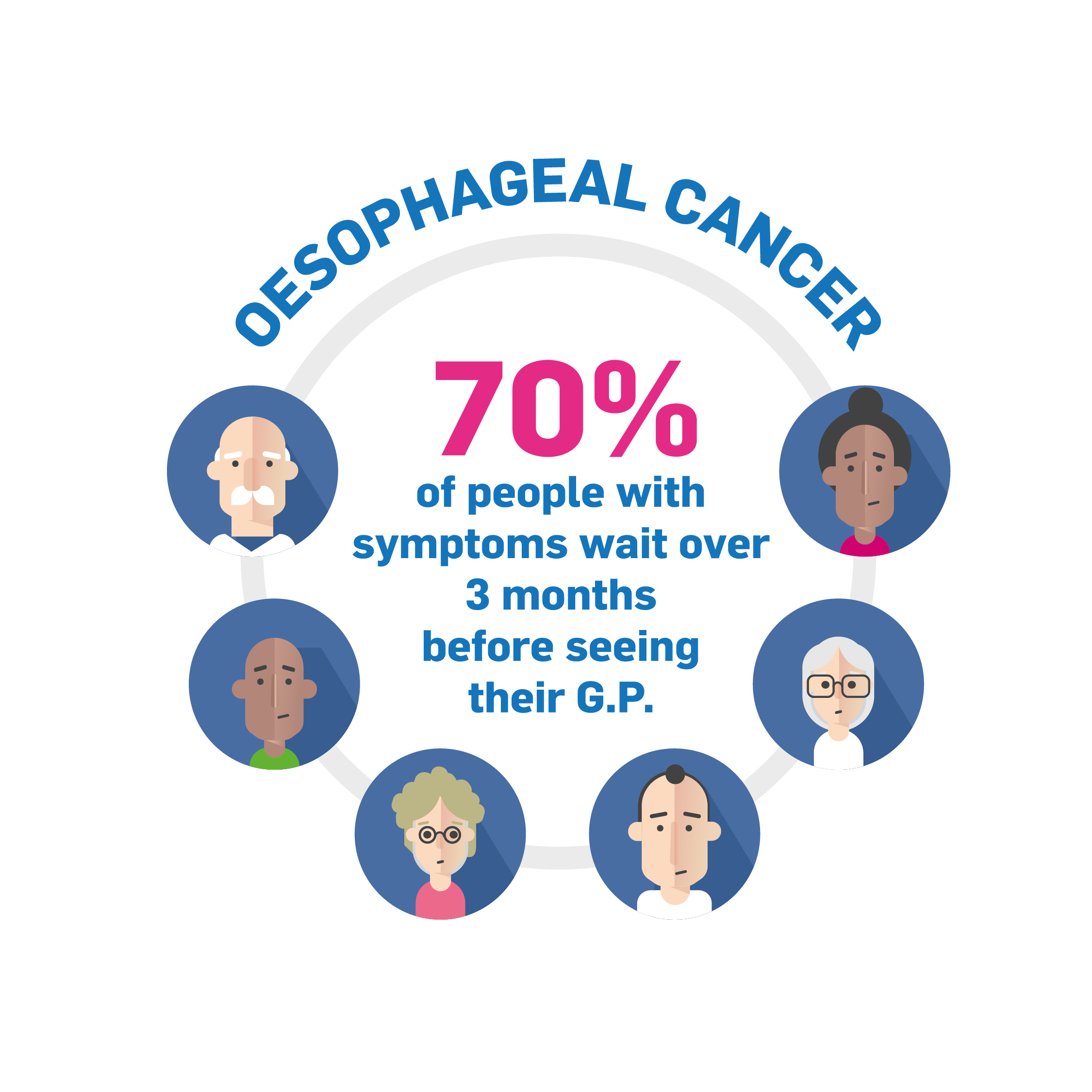
70% of patients with symptoms of Oesophageal Cancer wait over 3 months before seeking medical advice. It is important to seek medical advice if you are experiencing any of the symptoms of Oesophageal Cancer.
You should seek initial advice by making an appointment with your GP, you can explain your symptoms and your GP will conduct some examinations. This may include having blood tests, your GP may also refer you to see a specialist in hospital to have further tests.
You might have one or more of these tests so your doctors can find out the cause of your symptoms, or so they can find out the size of your cancer and whether it has spread. This tells you the stage of your cancer. Knowing the stage helps medical professionals decide which treatment you need.
Blood tests
Blood tests can be done by your GP or in hospital and you will be advised what tests you need and you can ask your doctor to tell you what they are checking for also.
Blood tests may include;
A full blood count - To check your red blood cells, white blood cells and platelet levels.
Organ function tests - to test how well your organs are working
Other blood tests - To check for example your protein or hormone levels as some cancers can produce chemicals that can be measured in the blood.
Your blood sample is sent to the laboratory for analysis. The analysis shows the different types of cells, chemicals and proteins in the blood.
Biopsy
While other tests can suggest that you may have cancer, only a biopsy can give a definitive diagnosis. A biopsy involves the removal of a small amount of tissue from an area where there are suspected abnormalities that can then go for examination.
The tissue sample is then sent to the laboratory for analysis.
A biopsy may be carried out during your endoscopy if the biopsy results show there are cancerous cells, you will discuss the options with your doctor at the hospital who will tell you what specialists you will be meeting.
These may include surgeons who specialise in Oesophageal cancers or doctors who specialise in treating Oesophageal Cancer. You may also see a specialist cancer nurse.
Endoscopy
An endoscopy is a test using a long flexible tube with a camera that examines the lining of your oesophagus for anything that looks abnormal or any growths in the area. Sedation is used during endoscopies where you will be given medication to become more relaxed or sleepy.
Endoscopies can also be used to take biopsies of any tissues in the oesophagus. These tissues are then tested to identify any abnormalities.
Following your endoscopy your doctor will speak to you about how the test went and the next steps. You should check how long they expect the results to take and who you should contact for the results. This may be the hospital or your GP.
If the biopsy results from your endoscopy show there are cancerous cells, your medical specialists may arrange for you to have more tests. These are organised to find out which layers of the oesophageal wall the cancer is in and if it has spread outside the oesophagus.
X-Ray, Barium Swallow, PET-CT Scan, CT Scan, MRI
An X-Ray uses a focused small amount of radiation to check inside the body for any abnormalities.
A special type of X-ray known as a Barium Swallow shows up parts of your digestive system, such as your oesophagus. You will be asked to drink a white chalky liquid called barium and x-rays are taken. The barium coats the oesophagus, making it easier for medical professionals to identify abnormalities or a tumor on the x-ray.
CT Scans take images of the inside of the body using x-rays, the images are taken from different angles they are then combined into a very detailed 3D picture. A CT scan allows medical professionals to check for any abnormalities or tumours. It also allows medical professionals to measure the size of a tumour if it is present, they may use a special dye, given to you before the scan to allow them to see more details.
A PET-CT uses both a PET scan and CT scan together. Creating a detailed picture of the organs and tissues inside the body. A PET scan uses a small amount of a radioactive sugar substance that is injected into the body. Cells that use a lot of energy take up the sugar substance, cancer cells tend to use a lot of energy so they absorb more of the sugar substance.
The PET scan then detects this substance to produce images of the inside of the body. A CT scan takes a series of detailed x-rays of the internal organs and tissues and combines them into a detailed 3D picture. During a PET-CT scan your doctors combine the two procedures to identify where exactly your Oesophageal Cancer is located and whether it has spread. It can also help doctors work out what tissues have been affected.
An MRI uses magnetic fields, not x-rays, to produce detailed images of the inside of the body. An MRI can be used to measure the size of a tumour. An injection may be administered before the procedure to highlight certain parts of the body to create a clearer picture for the medical professionals.
Endoscopic Ultrasound
An endoscopic ultrasound is an endoscopy using an ultrasound probe. It can produce more detailed pictures of the oesophagus and surrounding areas including lymph nodes.
This procedure is often done at the same time as the endoscopy. The ultrasound uses high frequency sound waves to provide images of the wall of the oesophagus as well as the lymph nodes and surrounding structures.
The ultrasound is often used to discover if a tumor has grown or whether the cancer has spread to the lymph nodes or other nearby areas. An ultrasound can also be used to help take a tissue sample from the lymph nodes.
Laparoscopy
You may have to have a laparoscopy if you have Oesophageal Cancer to check if the cancer has spread elsewhere. A laparoscopy is a small operation of the stomach to check inside your abdomen.
A laparoscopy is a thin tube with a light and a camera that is inserted through a small incision in the abdomen. Your doctor can then check the abdomen and take biopsies or tissue samples if needed.
Once you have had all of the tests your doctors will analyse the results and this information will help them determine the best treatment for you. Your doctors will explain the best treatment options for you and they will talk you through the treatment process and what you can expect from the different treatments and the possible side effects you may experience.
The treatment plan will be decided depending on:
The type of Oesophageal Cancer you have.
The stage and grade of the cancer such as the location of the cancer, the size of the tumor and whether it has spread
Your health at the time of diagnosis
Your personal decisions on treatment.
Once you have had all of the tests your doctors will analyse the results and this information will help them determine the location of the cancer, the size of the tumour, whether the cancer has spread and the type of Oesophageal Cancer for example whether it is adenocarcinoma (ACC) cancer that develops in the gland cells, for people who have been diagnosed with Oesophageal Cancer these cells produce the mucus in the lining of the oesophagus.
Or squamous cell carcinoma (SCC) cancer that develops from squamous cells that make up the inner lining of your oesophagus.
This process is called staging. Knowing the stage and grade helps your doctors plan the best treatment for you.Staging is a complicated process and your doctors will be able to provide you with more detailed information on your cancer diagnosis once they have all of the tests completed.
Staging is done clinically and pathologically.
Clinical staging involves your doctors determining the stage of Oesophageal Cancer from tests and scans.
Pathological staging involves staging an Oesophageal Cancer diagnosis following surgery.
Additionally doctors use the TNM staging process that refers to the tumour, node and metastasis.
This staging process describes;
T - the size of the tumour
N - whether the cancer has spread to the lymph nodes
M - whether the cancer has spread to any other parts of the body
Cancer Research UK have excellent resources explaining Oesophageal Cancer staging if you want to find out further information
https://www.cancerresearchuk.org/about-cancer/oesophageal-cancer/stages-types-and-grades
The results of your tests also help your doctors find out more about the grade of the Oesophageal Cancer diagnosis. The grade of cancer cells indicates how much the cancer cells look like normal cells and also gives your doctors an idea of how the cancer might grow and the type of treatment needed.
Knowing the grade of the cancer cells also helps your doctors plan the best treatment for you.
Cancer cells are graded from 1 to 3.
Grade 1 can be described as a low grade where the cancer cells look most like normal cells. It would be anticipated that these cancer cells would grow more slowly.
Grade 2 cancer cells look moderately like normal cells
Grade 3 or high grade cancer cells look more abnormal and not similar to normal cells. It would be expected that these cells would grow more quickly.

It can be a very overwhelming time when you receive an Oesophageal Cancer diagnosis. You might have received a lot of information from your doctors within a short period of time and you may want to know more information or you may be happy with the information you have right now and proceed on that basis.
For those struggling with making decisions during this time there are some things you might want to consider;
Do you need to make a quick decision, or could you take a short period of time such as overnight or a few days to process all of the information you have been given.
Do you have all of the information you need on the treatment you will be given.
Do you know all you need to know about what treatment can do for you.
Would you like to be connected with someone who has had a similar experience to you.
Do you have time to talk to family, friends or people close to you.
Do you need some time to think about your treatment options.
The Oesophageal Cancer Fund has some resources available for people who have just been diagnosed that can be accessed here
Your options may include:
Chemotherapy
Radiotherapy
Combination of Chemotherapy and Radiotherapy
Surgery
Chemotherapy
Chemotherapy works to destroy cancer cells using anti cancer drugs.
Depending on the type of chemotherapy administered it can be done intravenously into the bloodstream or in tablet form.
Your doctors will advise you on your exact treatment plan; You might have chemotherapy before or after surgery. You may have a combination of chemotherapy and radiotherapy (chemoradiotherapy) either before surgery or as your main treatment. Or you might have chemotherapy as your main treatment.
Your doctors will thoroughly explain when and where your treatment will take place and the cycle of treatments you may have.
Side effects of chemotherapy will also be explained to you. Some possible side effects associated with chemotherapy can include;
feeling tired
loss of appetite
feeling sick
nausea
diarrhoea or constipation
weight loss
susceptibility to infection
hair loss
Your doctors will be able to advise you on all of the side effects and ways to manage them and who to contact in the hospital if you have questions when you are at home.
Radiotherapy
Radiotherapy uses high energy rays that are directed specifically to destroy the cancer cells and maintain the surrounding healthy cells.
Your doctors will give you all of the information about your specific treatment plan. You might have radiotherapy combined with chemotherapy known as chemoradiotherapy. This may be given either before surgery. Alternatively you may have radiotherapy as your main treatment on its own as your main treatment.
Your doctors will thoroughly explain when and where your treatment will take place and the number of treatments you will have.
The side effects of radiotherapy will be explained to you but some of the side effects include;
feeling tired
skin reactions
feeling sick
Difficulty with eating radiotherapy can cause a sore throat and you may find it difficult to eat you will receive advice on this and treatment options available
hair loss
Your doctors will be able to advise you on all of the side effects and ways to manage them and who to contact in the hospital if you have questions when you are at home.
A PET-CT uses both a PET scan and CT scan together. Creating a detailed picture of the organs and tissues inside the body. A PET scan uses a small amount of a radioactive sugar substance that is injected into the body. Cells that use a lot of energy take up the sugar substance, cancer cells tend to use a lot of energy so they absorb more of the sugar substance.
The PET scan then detects this substance to produce images of the inside of the body. A CT scan takes a series of detailed x-rays of the internal organs and tissues and combines them into a detailed 3D picture. During a PET-CT scan your doctors combine the two procedures to identify where exactly your Oesophageal Cancer is located and whether it has spread. It can also help doctors work out what tissues have been affected.
An MRI uses magnetic fields, not x-rays, to produce detailed images of the inside of the body. An MRI can be used to measure the size of a tumour. An injection may be administered before the procedure to highlight certain parts of the body to create a clearer picture for the medical professionals.
Surgery
Surgery is a common treatment for cancer. Surgery for Oesophageal Cancer can include surgery to remove cancer from the lining of the oesophagus. Or for some people it may be necessary to remove part of the oesophagus or all of the oesophagus.
Your doctors will advise you on your exact surgery plan;
Endoscopic mucosal resection or EMR- surgery to remove cancer from the lining of the oesophagus.An EMR can be used to treat oesophageal cancer that is only in the inner lining of the oesophagus.
Your doctor will use an endoscope and pass surgical instruments through the endoscopic tube as well as fluid that is injected into the layer of cells below the cancer. The fluid highlights the cancer cells to allow them to be removed from the muscle layer of the oesophagus. The cells are removed using a small wire loop and suction.
Oesophagectomy
There are different types of surgery to remove the oesophagus. The type of surgery you have depends on the stage and position of the cancer.
You might have an oesophagectomy where part or all of your oesophagus is removed. Or an oesophago-gastrectomy where the surgery involves the removal of the top of your stomach and the part of your oesophagus where the cancer is located.
During surgery your doctor may also remove some of the nearby lymph nodes. This is known as a lymphadenectomy or lymph node dissection.
Surgery to remove Oesophageal Cancer are major operations. Your doctors will be able to advise you on all of the side effects of surgery and ways to manage them and who to contact in the hospital if you have questions when you are at home.
Combination of Chemotherapy and Radiotherapy
Chemoradiotherapy is a combined treatment of chemotherapy and radiotherapy.
Chemotherapy works to destroy cancer cells using anti cancer drugs.Radiotherapy uses high energy rays that are directed specifically to destroy the cancer cells and maintain the surrounding healthy cells.
Your doctors will advise you on your exact treatment plan;
You might have chemoradiotherapy either before surgery or as your main treatment. You also might start the chemotherapy before the radiotherapy starts and you may then continue to have chemotherapy during the radiotherapy treatment.
Side effects of chemotherapy will also be explained to you. Some possible side effects associated with chemotherapy can include;
feeling tired
loss of appetite
feeling sick
nausea
diarrhoea or constipation
weight loss
susceptibility to infection
hair loss
The side effects of radiotherapy will be explained to you but some of the side effects include;
feeling tired
skin reactions
feeling sick
Difficulty with eating radiotherapy can cause a sore throat and you may find it difficult to eat you will receive advice on this and treatment options available
hair loss
Your doctors will be able to advise you on all of the side effects and ways to manage them and who to contact in the hospital if you have questions when you are at home.
The Oesophageal Cancer Fund has other resources available for patients, carers and family that can be accessed here



